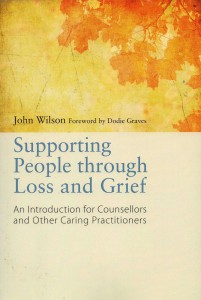
Because of some of the comments that have been made on Linkedin, about my assertion that Supporting People through Loss and Grief is a “Kübler-Ross free zone”, I feel that I may need to explain why. In fact Elisabeth Kübler-Ross is mentioned very briefly, on pages 81 and 82. There you will find it recounts Colin Murray Parkes’ story of how he met Kübler-Ross when in 1964 he was engaged in his famous Harvard Study of bereavement. There he discussed with the young trainee, the stages of grief he and John Bowlby had previously described. In 1961 they had described a three stage model: 1 yearning & searching. 2 disorganisation & despair, and 3 reorganisation. An earlier, 1952 three stage model of childhood distress: protest, despair and detachment, had been posited by John Bowlby and James Robertson, and it was this that gave rise to the stage model of grief. In 1970 Bowlby and Parkes published a four stage model, in which ‘numbness’ became the first stage and the other 1961 stages followed. When in 1969 Kübler-Ross published On Death and Dying, she introduced her now famous stages. As Colin Murray Parkes pointed out in the journal Mortality (2013, Vol. 18,No. 1, 94-97), Kübler-Ross made no mention of Parkes, Bowlby, or Robertson in her book, even in subsequent editions, and even though Colin Murray Parkes was generous enough to write the foreword to the 1970 British edition.
Consequently, many people continue to believe in the originality of the Kübler-Ross stages.
The other reason for a “Kübler-Ross free zone”, is the fact that her work is more about death and dying than about grief through bereavement, and her stages: denial, anger, bargaining, depression and acceptance, are about coming to terms with a terminal diagnosis, although many people, wrongly in my view, attribute them to stages of grief.
I rightly recognise the contribution to the field of palliative care made by Elisabeth Kübler-Ross. However, I believe that she has less to offer the field of bereavement than is widely believed.
You can find more about my book on this blog page.